Retinal Detachment
Definition
Retinal detachment is a separation of the retina from the underlying layer. This can lead to loss of peripheral and possibly central vision, depending on the extent of the retinal detachment.
Causes and Associations
There are three mechanisms of retinal detachment:
- Rhegmatogenous Retinal Detachment
Rhegmatogenous Retinal Detachment is caused by a break, tear or hole in the retina, allowing fluid from the center of the eye, or the vitreous cavity, to seep behind the retina and detach it. Rhegma is Greek for rent or break. Rhegmatogenous Retinal Detachment is the most common type of retinal detachment. Causes include trauma, separation of the vitreous from the retina, or prior intraocular surgery (e.g., cataract surgery). Nearsightedness is a risk factor for retinal tear and subsequent detachment. - Tractional Retinal Detachment
Tractional Retinal Detachment is caused by the pulling of membranes tethered to the retina. These membranous bands can be caused by diabetes mellitus, sickle cell disease, retinopathy of prematurity, or inflammatory conditions. - Exudative Retinal Detachment
Exudative Retinal Detachment is caused by fluid, or exudate, leaking from blood vessels underneath the retina. Causes include high blood pressure, vasculitis (inflammation of blood vessels), and tumors in the eye.
Symptoms
Patients with Rhegmatogenous Retinal Detachment are often presented with a shower of floaters (black dots or cobwebs in their vision), flashing lights, and a shadow, curtain, or cloud progressing from their peripheral vision.
Patients with Tractional Retinal Detachment may have flashing lights or a shadow over their vision, or they may have no symptoms.
Patients with Exudative Retinal Detachment have an area or darkness in their vision, which may shift with head position.
Examination
Complete and comprehensive ophthalmic examination is important in the assessment of retinal detachment. Patients will receive vision testing, drops to dilate pupils, and a complete examination of the front and back of the eye. Pupillary dilation may create blurring, and therefore, it is often best if a driver accompanies the patient, although it is not absolutely required. When examining the retina, the ophthalmologist may depress the eye with a cotton tip applicator or other blunt instrument in order to view the entire retina.
Examination & Testing
Patients with retinal detachment are largely diagnosed by clinical examination.
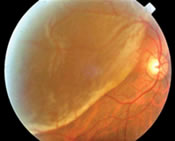
- Fundus Photography
Patients may undergo fundus photography to document the extent of retinal detachment. This procedure is of little risk to the patient. -
OCT Imaging
OCT imaging is a non-invasive optical coherence tomogram examination of the retina; an OCT uses low energy laser to scan the retina and determine whether there is fluid under the retina. It can help assess the status of retina and determine if there is a low lying retinal detachment.
What the Doctor Sees
In Rhegmatogenous Retinal Detachment, the ophthalmologist will see one or more breaks in the retina with underlying fluid. This can be accompanied by a vitreous hemorrhage, or bleeding into the central jelly of the eye.
In Tractional Retinal Detachment, there are membranous bands tethered to the retina causing a detachment. The pulling of these bands can lead to a retinal tear, owing to a combined rhegmatogenous and Tractional Retinal Detachment.
In Exudative Retinal Detachment, there is fluid under the retina in the absence of a retinal tear or a tethered band.
Prognosis
Retinal detachments were uniformly blinding until the first retinal detachment surgery was performed in the 1920’s. Surgical techniques have evolved since then, allowing good vision for many people with retinal detachment.
Retinal detachments can affect the peripheral and/or the central (i.e., macula) retina. Patients with peripheral retinal detachments can maintain excellent vision if the detachment is successfully repaired and it does not progress to involve the central retina. Patients with central, or macula-involving, retinal detachment can have decent but diminished vision if successfully repaired. Long-standing retinal detachments tend to have a poor visual prognosis.
Prevention
It is important to seek immediate ophthalmic care if one experiences symptoms of a retinal detachment, namely floaters, flashes, or a curtain over one’s vision. If the examining ophthalmologist discovers a retinal break or tear, he or she may refer you to a vitreoretinal surgeon. It may be possible to treat the tear with laser, known as retinopexy, or with a freezing treatment, known as cyrotherapy, to tack down the surrounding retina and prevent a retinal detachment.
Treatment
There are several modalities to treat a retinal detachment, dependant on the type, location, and size of the detachment:
- Pneumatic Retinopexy
Pneumatic retinopexy is an office procedure whereby a vitreoretinal specialist injects gas into the eye. This gas bubble helps block or tamponade a retinal tear, allowing the retinal pigment epithelium to pump out the subretinal fluid. Pneumatic retinopexy is coupled with either cryotherapy or laser retinopexy to tack down the retina surrounding the tear. When there is gas in the eye, patients must maintain appropriate head positioning to ensure the gas bubble abuts the retina tear. Also, patients with gas in their eye will be sensitive to significant changes in atmospheric pressure. They should not fly in a plane, mountain climb, or scuba dive until the gas bubble has resorbed. -
2. Scleral Buckle
A scleral buckle is a silicone band that surrounds and indents the eye to re-approximate the retinal detachment. It is coupled with cryotherapy or laser retinopexy. Patients will develop a cataract and become more nearsighted after this procedure. -
Intraocular Surgery/Vitrectomy
Patients with complicated tractional or exudative retinal detachments may require intraocular surgery (i.e., vitrectomy) removing the vitreous, or jelly, from the eye. This surgery allows removal of tractional bands tethered to the retinal. The surgeon may leave a gas bubble or silicone oil in the eye after vitrectomy to help reattach the retina.
Exudative retinal detachments are treated by addressing the underlying cause.